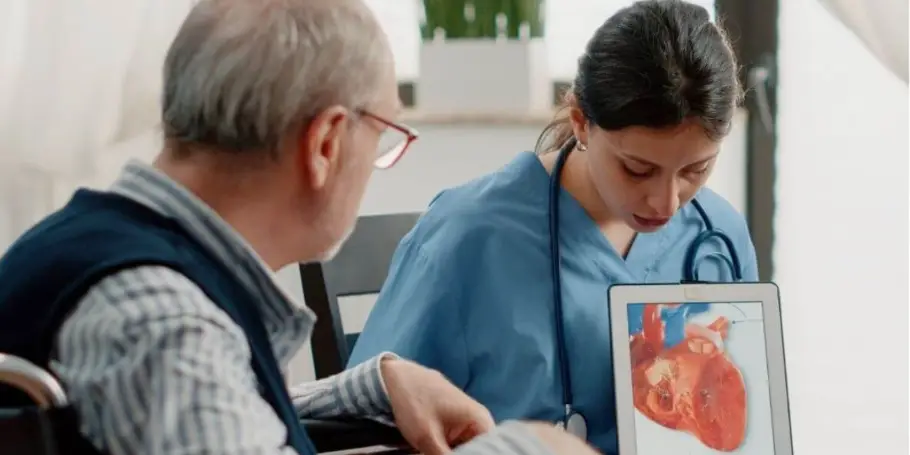
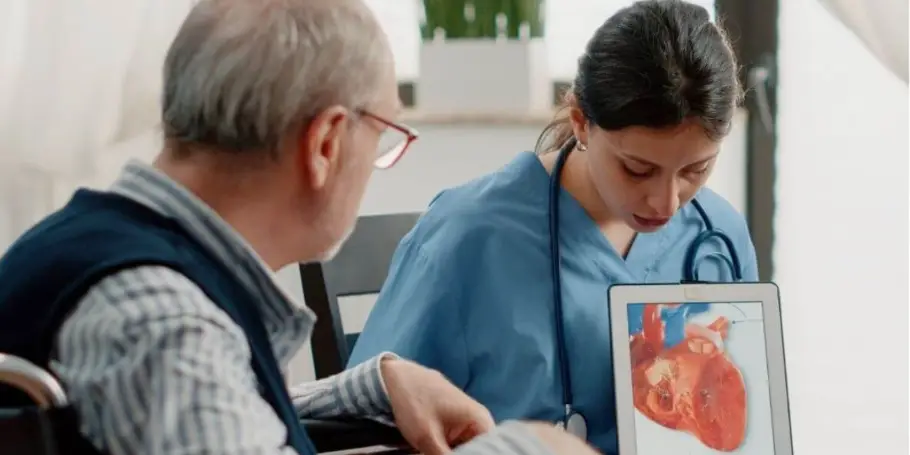
Heart Attack or Myocardial Infarction

Did you know that cardiovascular disease or heart disease, including a heart attack, is responsible for nearly 18 million deaths annually? That's almost one-third of all global deaths.
What is a heart attack?
A heart attack, or myocardial infarction (MI), occurs when blood flow to a part of the heart muscle is blocked for a prolonged period. This can damage or destroy part of the heart muscle.
The blockage is often due to a plaque in the coronary arteries. When this plaque ruptures, a blood clot forms, blocking the flow of blood. This interruption deprives the heart muscle of oxygen and nutrients, leading to heart muscle cells dying.
Common Causes of Heart Attacks
Atherosclerosis: Heart attacks are often triggered by atherosclerosis, the build-up of plaque in the coronary artery. This plaque, composed of fat, cholesterol, and other substances, can harden and narrow the arteries, restricting blood flow. When a plaque ruptures, a blood clot can form, completely blocking the artery and causing a heart attack.
High Cholesterol: High cholesterol levels significantly contribute to plaque build-up. Cholesterol can deposit on the artery walls, forming plaques that grow over time.
Blood Clots: Plaques that rupture can lead to blood clot formation. These clots can obstruct the flow of blood to the heart, causing a heart attack. Cardiac biomarkers, particularly troponin, play a crucial role in diagnosing myocardial infarction caused by such blood clots.
Smoking: Smoking damages the lining of the arteries, making it easier for plaque to build up and narrowing the arteries. It's a major risk factor for heart attacks.
Hypertension (High Blood Pressure): Hypertension forces the heart to work harder than normal, increasing the risk of heart attack. It can also damage the arteries, making them more susceptible to plaque build-up.
Other Factors: Obesity, diabetes, a sedentary lifestyle, and a poor diet also increase the risk of heart attacks. These factors can contribute to the development of atherosclerosis and other heart-related issues. Myocardial ischemia, resulting from insufficient blood flow to the heart muscle, can also occur due to these risk factors, leading to conditions such as acute coronary syndrome and acute myocardial infarction.
Heart Attack Symptoms and Signs
Chest Pain or Discomfort: The most frequent symptom is chest pain or discomfort. This may feel like pressure, squeezing, fullness, or pain that lasts for more than a few minutes or goes away and comes back.
Shortness of Breath: This can occur with or without chest discomfort and may make you feel like you can’t get enough air.
Nausea and Sweating: Some individuals experience nausea, vomiting, or cold sweats. These symptoms might be mistaken for other conditions but should never be ignored, especially when combined with other signs.
Dizziness: Feeling light-headed or dizzy is another possible symptom, often accompanied by chest pain or shortness of breath.
Jaw or Back Pain: Heart attack symptoms aren’t limited to the chest. Pain can spread to the jaw, back, neck, arms, or stomach. Sometimes, this pain might be mistaken for a muscle strain or other less serious condition.
Types of Myocardial Infarction
ST-Elevation Myocardial Infarction (STEMI): This is the most severe form of heart attack, characterised by a significant and sustained blockage of blood flow to the heart muscle. This type of myocardial infarction requires immediate medical attention due to the extensive damage it can cause.
Non-ST-Elevation Myocardial Infarction (NSTEMI): NSTEMI is a less severe form of heart attack compared to STEMI, but it still requires urgent medical treatment. In NSTEMI, the blockage of blood flow is partial or temporary, which means the damage to the heart muscle is usually less extensive.
Unstable Angina: This is another type of acute coronary syndromes that can lead to myocardial infarction if left untreated. It's characterised by chest pain or discomfort caused by narrowing of the coronary arteries, but without evidence of heart muscle damage.
Diagnosis of Myocardial Infarction
Electrocardiogram: An electrocardiogram (ECG) is a crucial test for suspected heart attacks, ideally performed within 10 minutes of hospital admission. It measures the heart's electrical activity, recording impulses on paper to assess heart function. The test is painless, takes about 5 minutes, and involves attaching electrodes to the arms, legs, and chest, which connect to the ECG machine.
Blood Tests: After a heart attack, specific proteins leak into the blood, indicating heart damage. Doctors test for these cardiac markers, particularly cardiac troponin, to diagnose the heart attack type.
Chest X-ray: A chest X-ray helps diagnose uncertain heart attacks and check for symptoms like pneumothorax. It also detects post-heart attack complications, such as pulmonary edema.
Echocardiogram: An echocardiogram uses sound waves to create an image of the heart, helping to identify damaged areas and assess their impact on heart function.
Coronary Angiography: Coronary angiography is a procedure used to detect blockages or narrowing in coronary arteries. It involves inserting a catheter into a blood vessel and guiding it to the coronary arteries using X-rays. A contrast agent is pumped through the catheter, and its flow is monitored to identify any blockages. This aids cardiologists in determining the best treatment.
Heart Attack Treatment Options
Immediate Emergency Treatment: Immediate action during a heart attack is vital. Key steps include performing CPR, using an AED, and calling emergency services. Quick and effective treatment is crucial to address potential cardiac arrest complications.
Medical Treatments: Medical treatments aim to restore heart blood flow and minimise damage. Key methods include angioplasty and stents to open arteries, thrombolytic drugs to dissolve clots, and bypass surgery like Coronary Artery Bypass Grafting (CABG) for severe cases.
Ongoing Treatments: Following a heart attack, ongoing care is vital for preventing future incidents and improving heart health. This involves taking medications like aspirin and statins, making lifestyle changes such as a heart-healthy diet and regular exercise, quitting smoking, and participating in cardiac rehabilitation programs.
How to prevent a heart attack?
Lifestyle Modifications: Adopting a heart-healthy lifestyle is vital to prevent heart attacks. This involves eating a balanced diet, exercising regularly, and avoiding smoking.
Managing Risk Factors: Managing risk factors is crucial for preventing heart attacks. Key strategies include controlling high blood pressure with medication, diet, and exercise; managing diabetes through blood sugar monitoring and lifestyle changes; and maintaining healthy cholesterol levels to prevent arterial plaque build-up.
Routine Heart Health Screenings: Regular check-ups are crucial for detecting and managing heart attack risk factors. Routine screenings like blood pressure, cholesterol, and blood sugar tests help identify issues early, allowing for timely intervention. Continuous monitoring is essential for maintaining heart health and preventing heart attacks.
When to seek medical help?

Swift action during a heart attack is crucial, as recognising symptoms and seeking immediate medical help can save lives.
Prince Court Medical Centre's Cardiology Department provides cutting-edge cardiac care with expert cardiologists offering personalised treatments and diagnostics. We focus on building trust and empowering patients for better heart health.